Color coding plays a vital role in the laboratory and in the clinic, especially in the blood collection process, to quickly distinguish test tube types and ensure the accuracy of sample processing. For example, **blood collection tube colour code** indicates the additive type and use of the tube by different colors, such as red tube for serum separation and purple tube for anticoagulant blood sample. This visual identification not only improves operational efficiency, but also reduces experimental or diagnostic errors caused by misuse of the tube. Next, we will analyze the color coding of various blood collection tubes and its specific meaning in detail to help you better understand and apply this key specification.
Color coding is used in blood collection to quickly identify the type of additive in the tube and the applicable test, ensuring the accuracy and efficiency of sample processing. The following are common blood collection tube colors and their uses:
 -Red: No additives or coagulants, often used for serum testing, such as biochemical analysis or blood type testing.
-Red: No additives or coagulants, often used for serum testing, such as biochemical analysis or blood type testing.
 - Purple: Contains EDTA anticoagulant, suitable for whole blood tests, such as blood routine or blood type analysis.
- Purple: Contains EDTA anticoagulant, suitable for whole blood tests, such as blood routine or blood type analysis.
 - Blue: Contains sodium citrate, mainly used for coagulation function tests, such as PT and APTT tests.
- Blue: Contains sodium citrate, mainly used for coagulation function tests, such as PT and APTT tests.
 - Yellow: contains separation glue and coagulant, is used for serum separation, and is suitable for immunology, endocrinology, and other tests.
- Yellow: contains separation glue and coagulant, is used for serum separation, and is suitable for immunology, endocrinology, and other tests.

Instructions for use of blood collection tubes(Black cap):
1. Main use
a) Black top blood tubes are mainly used to detect the ESR (Erythrocyte Sedimentation Rate), also known as the erythrocyte sedimentation rate.
b) This test is important for assessing the level of inflammation, infection, rheumatism and some other diseases in the body.
2. Additives
a) Black tubes usually contain sodium citrate as an anticoagulant, and its concentration ratio is generally 3.8%.
b) The function of sodium citrate is to prevent blood coagulation and maintain the liquid state of blood, which is convenient for ESR testing.
3. Specimen requirements
a) The collected blood should be fully mixed with the anticoagulant as required.
b) The test should be carried out as soon as possible after blood collection to ensure the accuracy of the results.
4. Tube design
a) The inner wall of the blood collection tube has been specially treated to prevent blood adhesion and ensure the anticoagulant effect.
b) The tube body usually has a capacity scale to facilitate the mixing of blood and anticoagulant in proportion.
5. Precautions
a) Avoid violent shaking during collection and transportation to avoid affecting the test results.
b) A dedicated ESR meter must be used for the test and the instrument needs to be calibrated for the specific anticoagulant concentration.
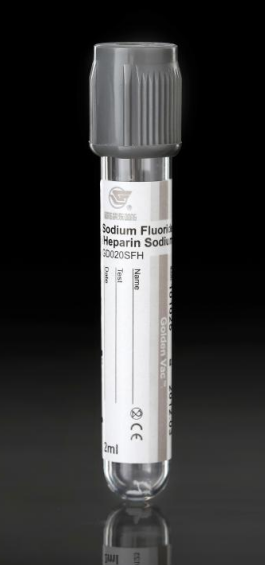
Blood collection tubes with gray caps (gray tubes) have their specific uses and characteristics among vacuum blood collection tubes and are mainly used for the detection of certain biochemical projects. The following is a detailed introduction:
1. Main uses
a) Gray tubes, commonly known as tubes for glucose testing, are primarily used for blood glucose analysis, especially in scenarios requiring control over blood glucose decomposition or metabolism.
b) It can also be used for the detection of metabolites such as lactate.
2. Additives
a) Gray tubes usually contain the following additives: Sodium fluoride: As a glucose metabolism inhibitor, it prevents blood glucose from decreasing due to metabolism after collection, ensuring that the measured blood glucose concentration is closer to the actual level.
b) EDTA or oxalate: used as an anticoagulant to prevent blood coagulation.
The role of additives is dual: on the one hand, it inhibits the decomposition of blood glucose, and on the other hand, it ensures that the specimen is anticoagulated for detection.
3. Usage characteristics
a) Anticoagulation and anti-metabolism: Gray tubes effectively inhibit the activity of enzymes by adding sodium fluoride, preventing red blood cells from continuing to metabolize glucose.
b) Time sensitivity: Especially suitable for tests that require accurate blood glucose values.
4. Operation requirements
a) After blood collection, gently invert and mix (5-8 times) to ensure that the blood and additives are fully in contact.
b) Centrifuge or store within the specified time to avoid specimen deterioration.
5. Specimen requirements
a) The test specimen should be processed as soon as possible after blood collection, usually refrigerated at 4°C to prolong the stability of the sample.
b) Before testing, care should be taken to avoid violent shaking or long-term exposure.
6. Precautions
a) The color of the blood collection tube must be accurately distinguished: the gray tube refers specifically to the blood collection tube containing sodium fluoride, and cannot be mixed with tubes for other purposes.
b) The blood glucose value tested may be slightly different from the results of other blood collection tubes (such as red tubes and green tubes) due to different metabolic inhibition effects.
Green tube blood collection tube is a type of vacuum blood collection tube commonly used in clinical practice. It is mainly used for biochemical project testing. The following is its detailed introduction:
1. Main purpose
Green tubes are usually used to detect biochemical indicators in blood, such as:
a) Electrolytes (sodium, potassium, chlorine, etc.)
b) Liver function (ALT, AST, bilirubin, etc.)
c) Kidney function (creatinine, urea nitrogen, etc.)
d) Blood gas analysis, etc.
2. Additives
The main additive in the green tube is heparin, as follows:
Sodium heparin or lithium heparin:
a) Heparin sodium: commonly used in general biochemical testing.
b) Lithium heparin: more common and suitable for plasma electrolyte testing because it does not significantly interfere with electrolyte levels such as sodium and potassium.
The additive works by inhibiting thrombin and coagulation factors by enhancing antithrombin III activity, thus preventing blood clotting.
3. Usage features
a) Rapid anticoagulation: Heparin has a rapid anticoagulant effect and is suitable for blood specimens that require rapid processing.
b) Applicable plasma: Separate plasma for testing after centrifugation.
4. Operational requirements
a) Mix well: After collecting blood, gently invert and mix (5-8 times) to avoid blood coagulation caused by uneven mixing.
b) Centrifugation processing: Plasma samples need to be centrifuged in time and stored refrigerated or frozen according to testing needs.
5. Specimen requirements
a) Testing items are differentiated according to specimen type: green tubes are mostly used for plasma testing and less for whole blood.
b) Not suitable for certain coagulation tests because heparin can interfere with coagulation test results.
6. Precautions
a) Moderate dosage of heparin: excessive amounts of additives may cause aggregation of white blood cells and platelets, interfering with detection.
b) Avoid repeated freezing and thawing: frozen specimens should be thawed and used once to avoid affecting the results.
This intuitive color classification reduces errors and ensures efficient and accurate diagnosis.